Detection of ascaris suum in the livers of chickens infected naturally by the nested multiplex PCR assay
This study was conducted to detect Ascaris suum, Toxocara canis,
and Toxocara cati in naturally infected chicken livers, and then to
provide information related to ascarid infections in humans. Ninetyfour chicken liver samples collected at a fresh market were used for
this study. DNA was extracted from each minced liver sample (500
mg) by the alkaline lysis method using NaOH 50mM and Tris-HCl
(pH 8.0). The nested multiplex PCR assay using ascarid universal
primers was applied to amplify the ITS1 ribosomal RNA gene of A.
suum, Toxocara canis, and Toxocara cati in all the liver samples.
Then, species specific-primers were used to discriminate between A.
suum and Toxocara spp. The results showed that 2 of the 94 chicken
liver samples detected positive for the presence of A. suum DNA.
This study provided useful information and evidence about A. suum
infection in humans via exposure to contaminated soil or eating
raw/undercooked chicken livers in Vietnam.
Trang 1

Trang 2

Trang 3
Trang 4
Trang 5
Trang 6
Tóm tắt nội dung tài liệu: Detection of ascaris suum in the livers of chickens infected naturally by the nested multiplex PCR assay

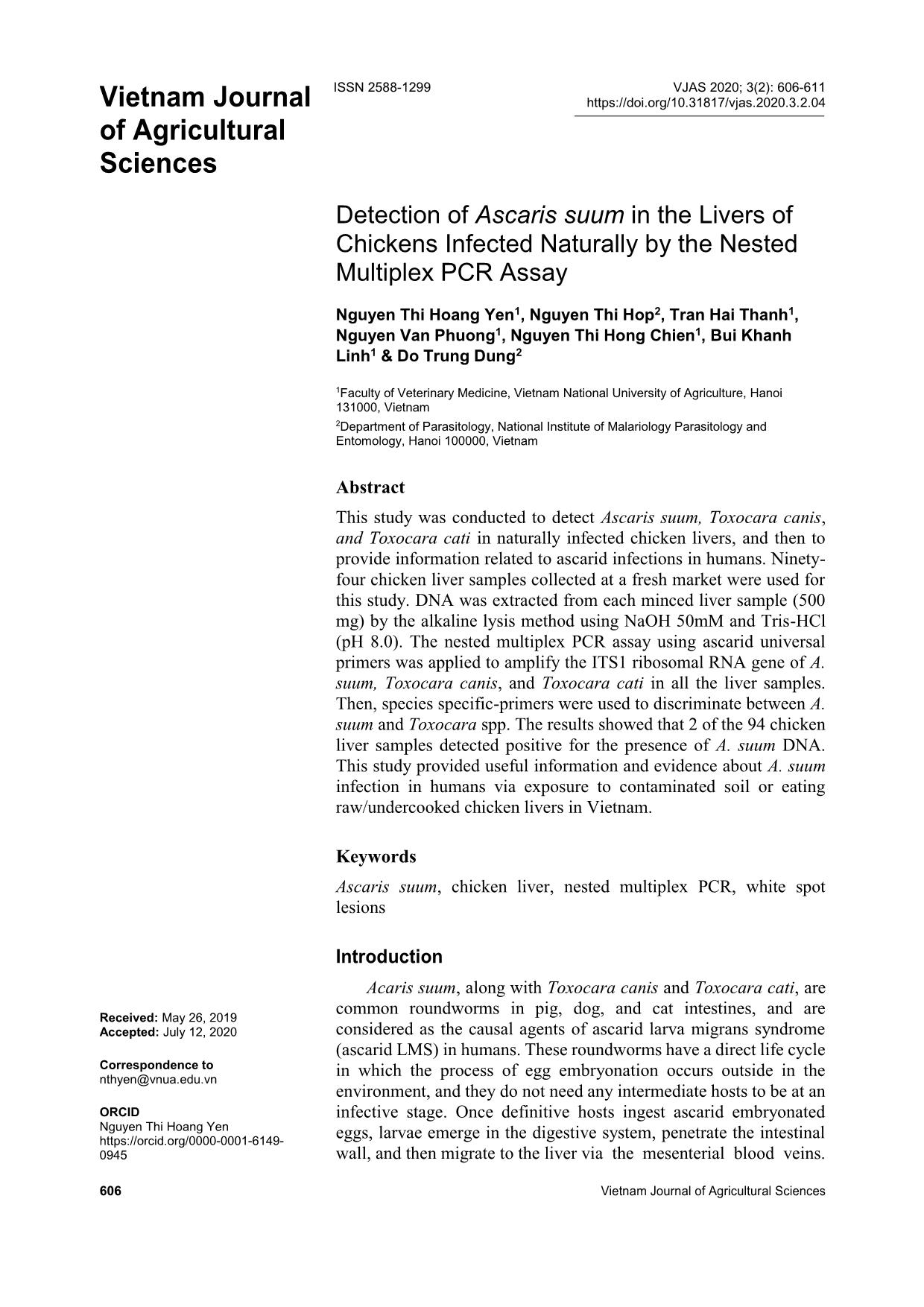
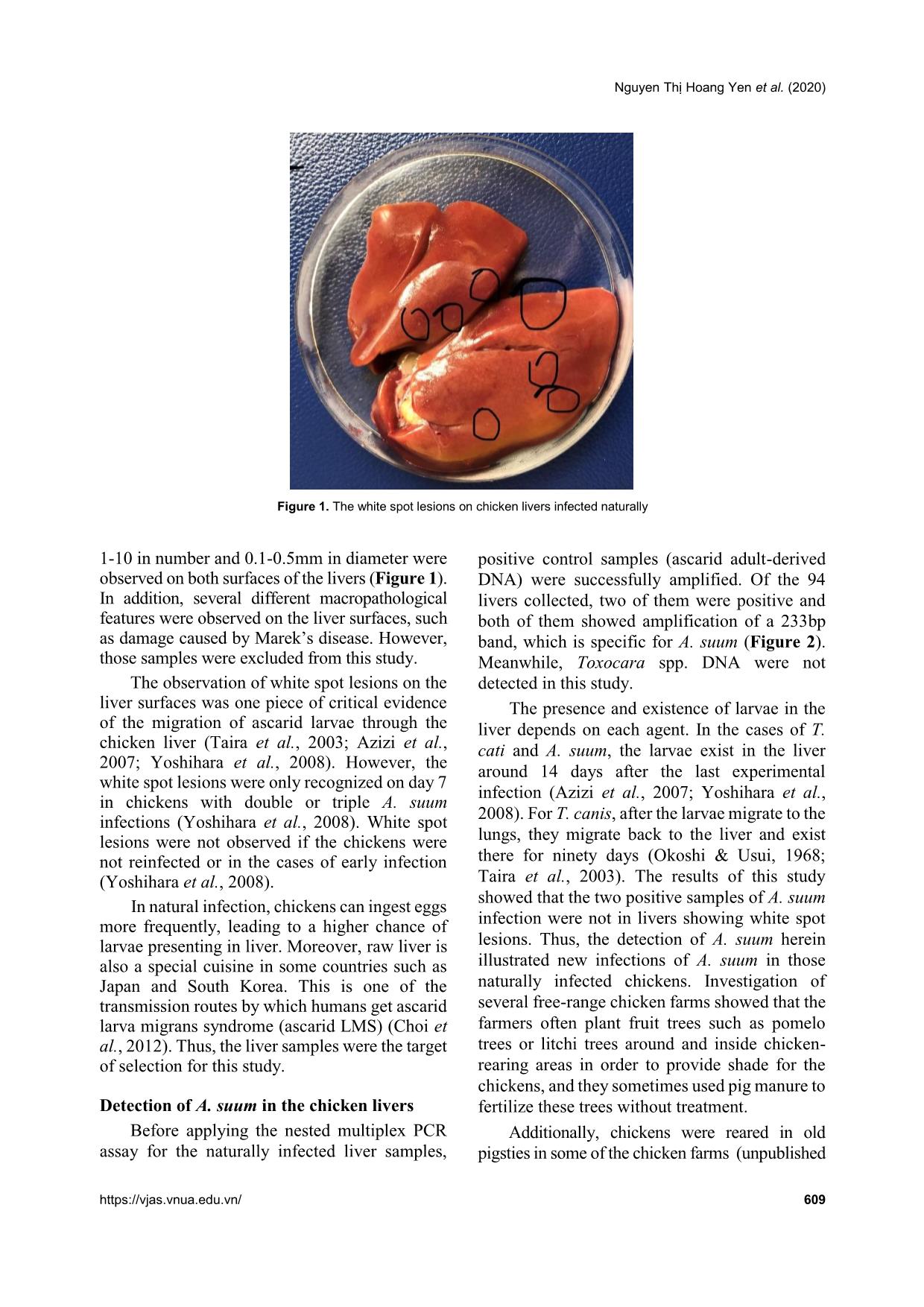
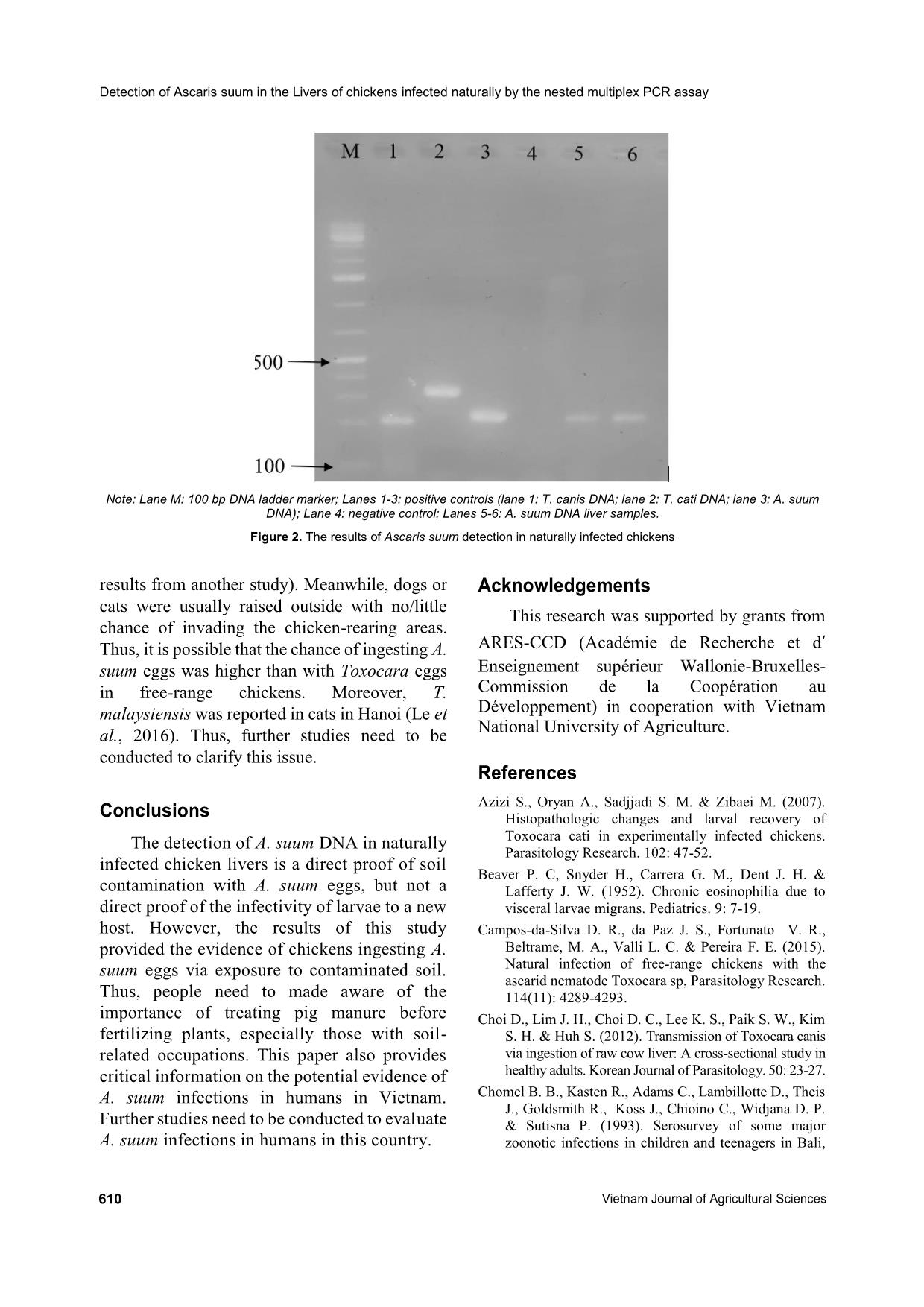
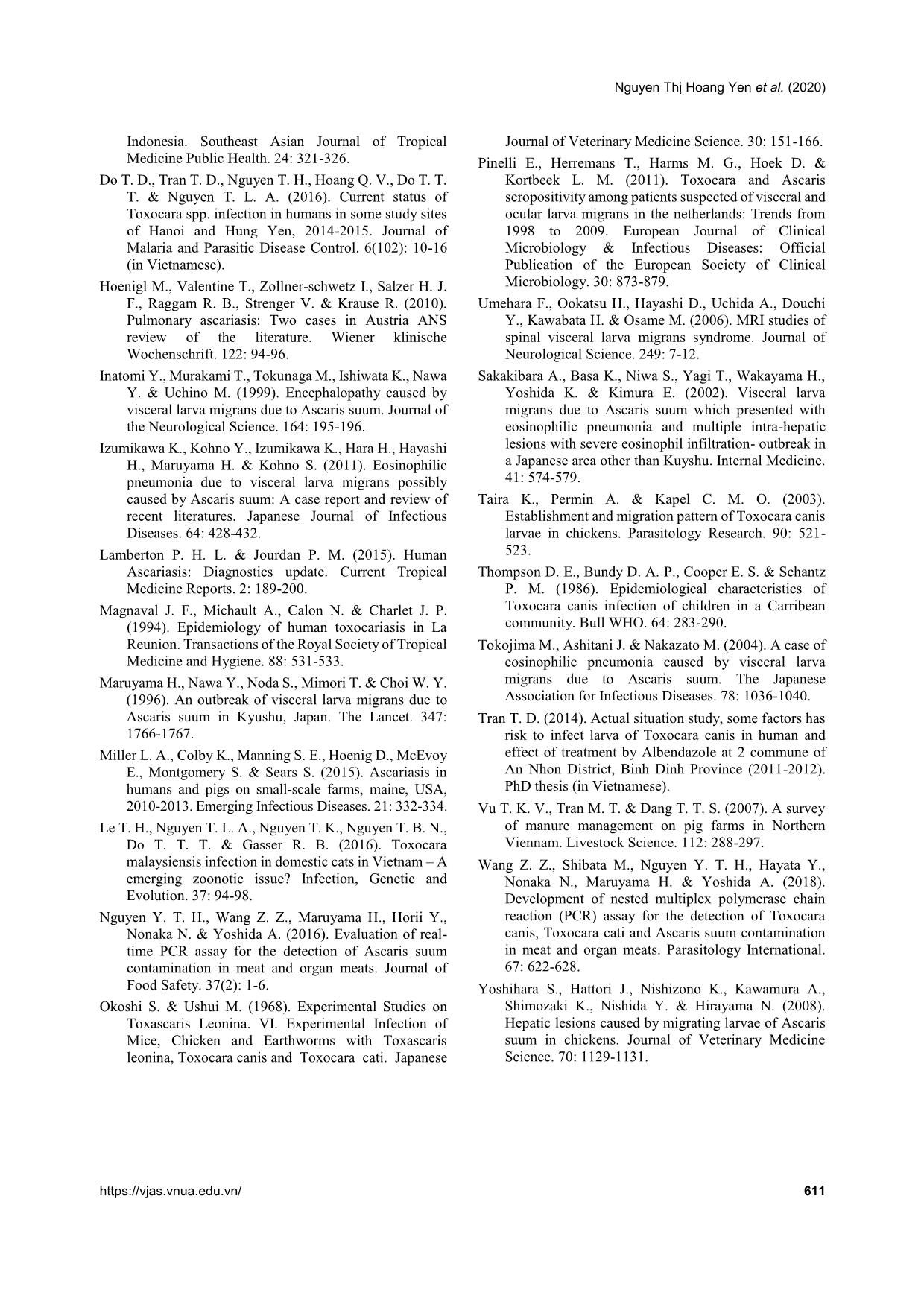
turally infected pigs, dogs, and cats, respectively, at local abattoirs around Hanoi. They were identified by morphology before performing the next steps. The roundworms were then thoroughly washed in saline solution and male worms were separated and kept in 70% alcohol for DNA extraction. Liver samples Ninety-four chickens were purchased from a fresh market in Trau Quy Town, Gia Lam district, Hanoi, Vietnam in order to collect the livers from naturally infected chickens. These free-range chickens were reared freely and derived from Hoa Binh, Bac Giang, and Hai Detection of Ascaris suum in the Livers of chickens infected naturally by the nested multiplex PCR assay 608 Vietnam Journal of Agricultural Sciences Duong provinces. The chickens then were necropsied to inspect the macropathology (white spot lesions) on the liver surfaces. Next, the livers were collected for the detection of A. suum by the nested multiplex PCR assay. DNA extraction The genomic DNA was extracted from adult A. suum, T. canis, and T. cati worms using a Blood- Animal- Plant preparation Kit (Jena Bioscience, Germany) following the manufacturer's instructions. DNA concentration was measured by NanoDrop 2000 (ThermoFisher Scientific, US) to detect the presence of DNA. The alkaline-lysis method was employed for extracting gDNA from the liver tissue. Five hundred milligrams (500mg) of chicken liver was homogenized in a 15mL tube provided by BioMasher (Nippi, Tokyo, Japan), and 1.8 mL of 50mM NaOH was added. After boiling for 30 min, the samples were neutralized by 200μL of 1M Tris-HCl (pH 8.0). The mixture was vortexed thoroughly and centrifuged at 14,000×g for 10min. The supernatant was transferred to a new tube and stored at -20°C until analysis (Nguyen et al., 2016). Nested multiplex PCR assay The nested multiplex PCR assay was applied to amplify a region of the ITS1 ribosomal RNA gene of A. suum, T. canis, and T. cati. The PCR reaction was performed in the total volume of 25 μl containing 1μL of template DNA and the following PCR mixture: 12.5μL Master mix 2X (Phusa Biochem, Vietnam), 0.75μL of each primer at concentrations of 0.3mM (Phusa Biochem, Vietnam) and 10μL distilled water. The thermal cycling profile was 94°C for 2min, followed by 40 cycles with denaturation at 94°C for 15s, primer annealing at 52°C for 30s, and extending at 68°C for 1min, and a final elongation step at 72oC for 7min. The first PCR products were used as a template in the species- specific nested multiplex PCR, in which multiple primer sets were applied in the same tube with 0.75μL of each of species-specific forward and reverse at concentrations 0.3mM. The PCR conditions were similar to the first reaction, except for primer annealing was at 57oC (Table 1) (Wang et al., 2018). The amplification products were analyzed using 1.0% agarose gel electrophoresis. The amplification bands were visualized under UV light. A positive reaction was observed when the appearance of the specific sized bands of 208bp, 325bp, and 233bp corresponding with T. canis, T. cati, and A. suum, respectively (Wang et al., 2018). Results and Discussion Macroscopic inspection on the liver surfaces Most of the collected livers were normal in color and structure. However, 15 of the 94 chickens showed macropathological damage on their livers. White spot lesions ranging from Table 1. Primer sequences that were used for the nested PCR and nested multiplex PCR (Wang et al., 2018) Primers Sequences Ascarid specific universal Primers (First PCR) Ascarid Forward: 5’-CGTCGGTAGCGATGAAAGGT-3’ Reverse: 5’-TTAGTTTCTTTTCCTCCGCT-3’ Species-specific primers (second PCR) T. canis Forward: 5’-CTCGAGTCGACGAAGTATGTAC-3’ Reverse: 5’-AATTGGGCCGCCCATCATAC-3’ T. cati Forward: 5’-GTAAGATCGTGGCACGCGTACGTA-3’ Reverse: 5’-TCTTTGATGTCAAGACTTCAGCGC-3’ A. suum Forward: 5’-TCAACATTCATAGAGAATGGCATGT-3’ Reverse: 5’-TACATCATTATTGTCACGCTCATCT-3’ Nguyen Thị Hoang Yen et al. (2020) https://vjas.vnua.edu.vn/ 609 Figure 1. The white spot lesions on chicken livers infected naturally 1-10 in number and 0.1-0.5mm in diameter were observed on both surfaces of the livers (Figure 1). In addition, several different macropathological features were observed on the liver surfaces, such as damage caused by Marek’s disease. However, those samples were excluded from this study. The observation of white spot lesions on the liver surfaces was one piece of critical evidence of the migration of ascarid larvae through the chicken liver (Taira et al., 2003; Azizi et al., 2007; Yoshihara et al., 2008). However, the white spot lesions were only recognized on day 7 in chickens with double or triple A. suum infections (Yoshihara et al., 2008). White spot lesions were not observed if the chickens were not reinfected or in the cases of early infection (Yoshihara et al., 2008). In natural infection, chickens can ingest eggs more frequently, leading to a higher chance of larvae presenting in liver. Moreover, raw liver is also a special cuisine in some countries such as Japan and South Korea. This is one of the transmission routes by which humans get ascarid larva migrans syndrome (ascarid LMS) (Choi et al., 2012). Thus, the liver samples were the target of selection for this study. Detection of A. suum in the chicken livers Before applying the nested multiplex PCR assay for the naturally infected liver samples, positive control samples (ascarid adult-derived DNA) were successfully amplified. Of the 94 livers collected, two of them were positive and both of them showed amplification of a 233bp band, which is specific for A. suum (Figure 2). Meanwhile, Toxocara spp. DNA were not detected in this study. The presence and existence of larvae in the liver depends on each agent. In the cases of T. cati and A. suum, the larvae exist in the liver around 14 days after the last experimental infection (Azizi et al., 2007; Yoshihara et al., 2008). For T. canis, after the larvae migrate to the lungs, they migrate back to the liver and exist there for ninety days (Okoshi & Usui, 1968; Taira et al., 2003). The results of this study showed that the two positive samples of A. suum infection were not in livers showing white spot lesions. Thus, the detection of A. suum herein illustrated new infections of A. suum in those naturally infected chickens. Investigation of several free-range chicken farms showed that the farmers often plant fruit trees such as pomelo trees or litchi trees around and inside chicken- rearing areas in order to provide shade for the chickens, and they sometimes used pig manure to fertilize these trees without treatment. Additionally, chickens were reared in old pigsties in some of the chicken farms (unpublished Detection of Ascaris suum in the Livers of chickens infected naturally by the nested multiplex PCR assay 610 Vietnam Journal of Agricultural Sciences Note: Lane M: 100 bp DNA ladder marker; Lanes 1-3: positive controls (lane 1: T. canis DNA; lane 2: T. cati DNA; lane 3: A. suum DNA); Lane 4: negative control; Lanes 5-6: A. suum DNA liver samples. Figure 2. The results of Ascaris suum detection in naturally infected chickens results from another study). Meanwhile, dogs or cats were usually raised outside with no/little chance of invading the chicken-rearing areas. Thus, it is possible that the chance of ingesting A. suum eggs was higher than with Toxocara eggs in free-range chickens. Moreover, T. malaysiensis was reported in cats in Hanoi (Le et al., 2016). Thus, further studies need to be conducted to clarify this issue. Conclusions The detection of A. suum DNA in naturally infected chicken livers is a direct proof of soil contamination with A. suum eggs, but not a direct proof of the infectivity of larvae to a new host. However, the results of this study provided the evidence of chickens ingesting A. suum eggs via exposure to contaminated soil. Thus, people need to made aware of the importance of treating pig manure before fertilizing plants, especially those with soil- related occupations. This paper also provides critical information on the potential evidence of A. suum infections in humans in Vietnam. Further studies need to be conducted to evaluate A. suum infections in humans in this country. Acknowledgements This research was supported by grants from ARES-CCD (Académie de Recherche et d’ Enseignement supérieur Wallonie-Bruxelles- Commission de la Coopération au Développement) in cooperation with Vietnam National University of Agriculture. References Azizi S., Oryan A., Sadjjadi S. M. & Zibaei M. (2007). Histopathologic changes and larval recovery of Toxocara cati in experimentally infected chickens. Parasitology Research. 102: 47-52. Beaver P. C, Snyder H., Carrera G. M., Dent J. H. & Lafferty J. W. (1952). Chronic eosinophilia due to visceral larvae migrans. Pediatrics. 9: 7-19. Campos-da-Silva D. R., da Paz J. S., Fortunato V. R., Beltrame, M. A., Valli L. C. & Pereira F. E. (2015). Natural infection of free-range chickens with the ascarid nematode Toxocara sp, Parasitology Research. 114(11): 4289-4293. Choi D., Lim J. H., Choi D. C., Lee K. S., Paik S. W., Kim S. H. & Huh S. (2012). Transmission of Toxocara canis via ingestion of raw cow liver: A cross-sectional study in healthy adults. Korean Journal of Parasitology. 50: 23-27. Chomel B. B., Kasten R., Adams C., Lambillotte D., Theis J., Goldsmith R., Koss J., Chioino C., Widjana D. P. & Sutisna P. (1993). Serosurvey of some major zoonotic infections in children and teenagers in Bali, Nguyen Thị Hoang Yen et al. (2020) https://vjas.vnua.edu.vn/ 611 Indonesia. Southeast Asian Journal of Tropical Medicine Public Health. 24: 321-326. Do T. D., Tran T. D., Nguyen T. H., Hoang Q. V., Do T. T. T. & Nguyen T. L. A. (2016). Current status of Toxocara spp. infection in humans in some study sites of Hanoi and Hung Yen, 2014-2015. Journal of Malaria and Parasitic Disease Control. 6(102): 10-16 (in Vietnamese). Hoenigl M., Valentine T., Zollner-schwetz I., Salzer H. J. F., Raggam R. B., Strenger V. & Krause R. (2010). Pulmonary ascariasis: Two cases in Austria ANS review of the literature. Wiener klinische Wochenschrift. 122: 94-96. Inatomi Y., Murakami T., Tokunaga M., Ishiwata K., Nawa Y. & Uchino M. (1999). Encephalopathy caused by visceral larva migrans due to Ascaris suum. Journal of the Neurological Science. 164: 195-196. Izumikawa K., Kohno Y., Izumikawa K., Hara H., Hayashi H., Maruyama H. & Kohno S. (2011). Eosinophilic pneumonia due to visceral larva migrans possibly caused by Ascaris suum: A case report and review of recent literatures. Japanese Journal of Infectious Diseases. 64: 428-432. Lamberton P. H. L. & Jourdan P. M. (2015). Human Ascariasis: Diagnostics update. Current Tropical Medicine Reports. 2: 189-200. Magnaval J. F., Michault A., Calon N. & Charlet J. P. (1994). Epidemiology of human toxocariasis in La Reunion. Transactions of the Royal Society of Tropical Medicine and Hygiene. 88: 531-533. Maruyama H., Nawa Y., Noda S., Mimori T. & Choi W. Y. (1996). An outbreak of visceral larva migrans due to Ascaris suum in Kyushu, Japan. The Lancet. 347: 1766-1767. Miller L. A., Colby K., Manning S. E., Hoenig D., McEvoy E., Montgomery S. & Sears S. (2015). Ascariasis in humans and pigs on small-scale farms, maine, USA, 2010-2013. Emerging Infectious Diseases. 21: 332-334. Le T. H., Nguyen T. L. A., Nguyen T. K., Nguyen T. B. N., Do T. T. T. & Gasser R. B. (2016). Toxocara malaysiensis infection in domestic cats in Vietnam – A emerging zoonotic issue? Infection, Genetic and Evolution. 37: 94-98. Nguyen Y. T. H., Wang Z. Z., Maruyama H., Horii Y., Nonaka N. & Yoshida A. (2016). Evaluation of real- time PCR assay for the detection of Ascaris suum contamination in meat and organ meats. Journal of Food Safety. 37(2): 1-6. Okoshi S. & Ushui M. (1968). Experimental Studies on Toxascaris Leonina. VI. Experimental Infection of Mice, Chicken and Earthworms with Toxascaris leonina, Toxocara canis and Toxocara cati. Japanese Journal of Veterinary Medicine Science. 30: 151-166. Pinelli E., Herremans T., Harms M. G., Hoek D. & Kortbeek L. M. (2011). Toxocara and Ascaris seropositivity among patients suspected of visceral and ocular larva migrans in the netherlands: Trends from 1998 to 2009. European Journal of Clinical Microbiology & Infectious Diseases: Official Publication of the European Society of Clinical Microbiology. 30: 873-879. Umehara F., Ookatsu H., Hayashi D., Uchida A., Douchi Y., Kawabata H. & Osame M. (2006). MRI studies of spinal visceral larva migrans syndrome. Journal of Neurological Science. 249: 7-12. Sakakibara A., Basa K., Niwa S., Yagi T., Wakayama H., Yoshida K. & Kimura E. (2002). Visceral larva migrans due to Ascaris suum which presented with eosinophilic pneumonia and multiple intra-hepatic lesions with severe eosinophil infiltration- outbreak in a Japanese area other than Kuyshu. Internal Medicine. 41: 574-579. Taira K., Permin A. & Kapel C. M. O. (2003). Establishment and migration pattern of Toxocara canis larvae in chickens. Parasitology Research. 90: 521- 523. Thompson D. E., Bundy D. A. P., Cooper E. S. & Schantz P. M. (1986). Epidemiological characteristics of Toxocara canis infection of children in a Carribean community. Bull WHO. 64: 283-290. Tokojima M., Ashitani J. & Nakazato M. (2004). A case of eosinophilic pneumonia caused by visceral larva migrans due to Ascaris suum. The Japanese Association for Infectious Diseases. 78: 1036-1040. Tran T. D. (2014). Actual situation study, some factors has risk to infect larva of Toxocara canis in human and effect of treatment by Albendazole at 2 commune of An Nhon District, Binh Dinh Province (2011-2012). PhD thesis (in Vietnamese). Vu T. K. V., Tran M. T. & Dang T. T. S. (2007). A survey of manure management on pig farms in Northern Viennam. Livestock Science. 112: 288-297. Wang Z. Z., Shibata M., Nguyen Y. T. H., Hayata Y., Nonaka N., Maruyama H. & Yoshida A. (2018). Development of nested multiplex polymerase chain reaction (PCR) assay for the detection of Toxocara canis, Toxocara cati and Ascaris suum contamination in meat and organ meats. Parasitology International. 67: 622-628. Yoshihara S., Hattori J., Nishizono K., Kawamura A., Shimozaki K., Nishida Y. & Hirayama N. (2008). Hepatic lesions caused by migrating larvae of Ascaris suum in chickens. Journal of Veterinary Medicine Science. 70: 1129-1131.
File đính kèm:
 detection_of_ascaris_suum_in_the_livers_of_chickens_infected.pdf
detection_of_ascaris_suum_in_the_livers_of_chickens_infected.pdf